Hemochromatosis
Hemocromatose
DOI:
https://doi.org/10.24950/rspmi.2578Keywords:
Hemocromatose/classificação, Hemocromatose/ diagnóstico, Hemocromatose/epidemiologia, Hemocromatose/ fisiopatologia, Hemocromatose/terapiaAbstract
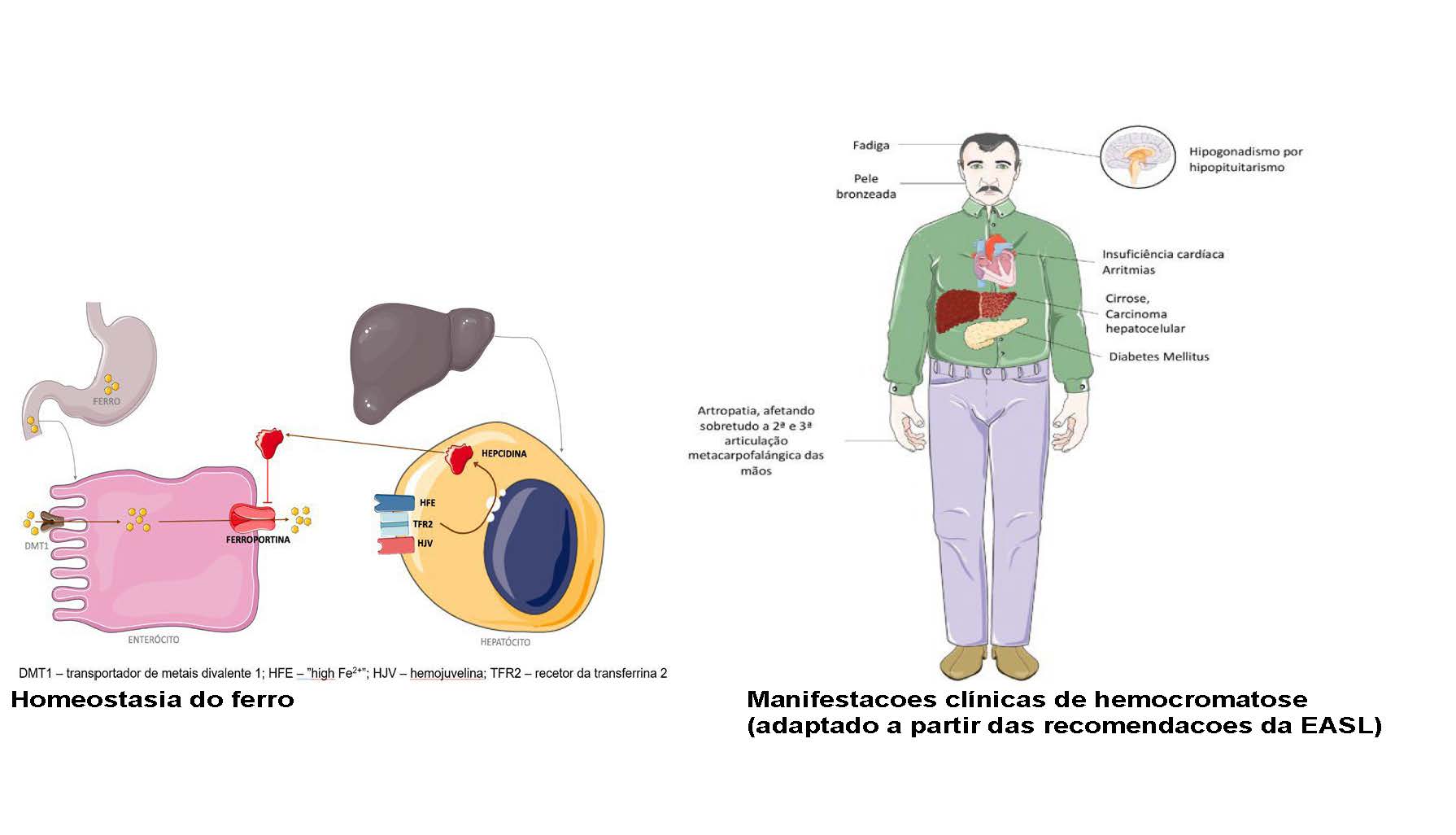
A hemocromatose é uma doença hereditária do metabolismo do ferro que resulta de defeitos genéticos no eixo hepcidina-ferroportina, com penetrância variável e, portanto, heterogeneidade clínica. Ocorre uma absorção descontrolada do ferro e risco de sobrecarga a nível do fígado, coração, pâncreas, articulações e órgãos endócrinos. Os doentes estão em risco de evolução para cirrose e carcinoma hepático. Deve ser suspeitada na presença de sintomas, história familiar ou elevação dos marcadores séricos do ferro, em especial da saturação da transferrina. O diagnóstico é desafiante pela inespecificidade de manifestações clínicas e dos marcadores séricos do ferro. Há vários genes implicados,
mas o HFE é o mais frequentemente afetado; a homozigotia C282Y associada a sobrecarga de ferro faz diagnóstico; outras variantes genéticas podem necessitar de estudo complementar com ressonância magnética ou biópsia hepática. O tratamento preferencial é a flebotomia, ou, em alternativa, eritrocitaferese ou quelação do ferro. Apresentam elevada morbimortalidade que pode ser reduzida com o início atempado do tratamento.
Downloads
References
Kowdley KV, Brown KE, Ahn J, Sundaram V. ACG Clinical Guideline: Hereditary Hemochromatosis. Am J Gastroenterol. 2019;114:1202-18. doi: 10.14309/ajg.0000000000000315. Erratum in: Am J Gastroenterol. 2019;114:1927. doi: 10.14309/ajg.0000000000000469.
Zoller H, Schaefer B, Vanclooster A, Griffiths B, Bardou-Jacquet E, Corradini E, et al. EASL Clinical Practice Guidelines on haemochromatosis. 2022.
Girelli D, Busti F, Brissot P, Cabantchik I, Muckenthaler MU, Porto G. Hemochromatosis classification: update and recommendations by the BIOIRON Society. Blood. 2022;139:3018-29. doi: 10.1182/blood.2021011338.
Bacon BR, Adams PC, Kowdley KV, Powell LW, Tavill AS. Diagnosis and Management of Hemochromatosis: 2011 Practice Guideline by the American Association for the Study of Liver Diseases. Hepatology. 2011;54:328- 43. doi: 10.1002/hep.24330.
Olynyk JK, Cullen DJ, Aquilia S, Rossi E, Summerville L, Powell LW. A Population-Based Study of the Clinical Expression of the Hemochromatosis Gene. N Engl J Med. 1999;341:718-24. doi: 10.1056/NEJM199909023411002.
Merryweather-Clarke AT, Pointon JJ, Shearman JD, Robson KJ. Global prevalence of putative haemochromatosis mutations. J Med Genet. 1997;34:275-8. doi: 10.1136/jmg.34.4.275.
Cardoso CS, Oliveira P, Porto G, Oberkanins C, Mascarenhas M, Rodrigues P, et al. Comparative study of the two more frequent HFE mutations (C282Y and H63D): significant different allelic frequencies between the North and South of Portugal. Eur J Hum Genet. 2001;9:843-8. doi: 10.1038/sj.ejhg.5200723.
Wallace DF, Subramaniam VN. The global prevalence of HFE and non-HFE hemochromatosis estimated from analysis of next-generation sequencing data. Genet Med. 2016;18:618-26. doi: 10.1038/gim.2015.140.
Allen KJ, Gurrin LC, Constantine CC, Osborne NJ, Delatycki MB, Nicoll AJ. Iron-overload–related disease in HFE hereditary hemochromatosis. N Engl J Med. 2008;358:221-30. doi: 10.1056/NEJMoa073286.
Adams PC, Jeffrey G, Ryan J. Haemochromatosis. Lancet. 2023; 27;401:1811-21. doi: 10.1016/S0140-6736(23)00287-8.
Olynyk JK, Ramm GA. Hemochromatosis. N Engl J Med. 2022;387:2159-70. doi: 10.1056/NEJMra2119758.
Nemeth E, Ganz T. Hepcidin and iron in health and disease. Annu Rev Med.2023;27:74 : 261-77. doi: 10.1146/annurev-med-043021-032816.
Cabrera E, Crespo G, VanWagner LB. Diagnosis and management of hereditary hemochromatosis. JAMA. 2022;328:1862-3. doi: 10.1001/jama.2022.17727.
Andersson L, Powell LW, Ramm LE, Ramm GA, Olynyk JK. Arthritis prediction of advanced hepatic fibrosis in HFE hemochromatosis. Mayo Clin Proc. 2022;97:1649-55. doi: 10.1016/j.mayocp.2022.02.017.
Legros L, Bardou-Jacquet E, Latournerie M, Guillygomarc'h A, Turlin B, Lan CL, et al. Non-invasive assessment of liver fibrosis in C282Y homozygous HFE hemochromatosis. Liver Int. 2015;35:1731-8. doi: 10.1111/liv.12762.
Crawford DH, Ramm GA, Bridle KR, Nicoll AJ, Delatycki MB, Olynyk JK. Clinical practice guidelines on hemochromatosis: Asian Pacific Association for the Study of the Liver. Hepatol Int. 2023;17:522-41. doi: 10.1007/s12072-023-10510-3.
Bardou-Jacquet E, Hamdi-Roze H, Paisant A, Decraecker M, Bourlière M, Ganne-Carrié N, et al. Non-invasive diagnosis and follow-up of hyperferritinaemia. Clin Res Hepatol Gastroenterol. 2022;46:101762. doi: 10.1016/j.clinre.2021.101762.
Cancado RD, Alvarenga A, Santos P. HFE hemochromatosis: an overview about therapeutic recommendations. Hematol Transfus Cell Ther. 2022; 44:95-9. doi: 10.1016/j.htct.2021.06.020.
Osborne NJ, Gurrin LC, Allen KJ, Constantine CC, Delatycki MB, McLaren CE. HFEC282Y Homozygotes Are at Increased Risk ofBreast and Colorectal Cancer. Hepatology. 2010;51:1311-8. doi: 10.1002/hep.23448.
Atkins JL, Pilling LC, Masoli JAH, Kuo CL, Shearman JD, Adams PC. Association of hemochromatosis HFE p.C282Y homozygosity with hepatic malignancy. JAMA. 2020;324: 2048-57. doi: 10.1001/jama.2020.21566.
Downloads
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2024 Internal Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright (c) 2023 Medicina Interna





