Direct Costs of Heart Failure in the Autonomous Region of Madeira
Custos Diretos da Insuficiência Cardíaca na Região Autónoma da Madeira
DOI:
https://doi.org/10.24950/rspmi.1778Keywords:
Custo da Doença, Despesas de Saúde, Ilha da Madeira, Insuficiência Cardíaca/economia, PortugalAbstract
Introdução: A insuficiência cardíaca (IC) é um problema
global de saúde pública. Desconhece-se o impacto económico da IC na Região Autónoma da Madeira (RAM) pelo que é fundamental caracterizar a sua prevalência, perfil de utilização de recursos e custos associados.
O nosso objetivo foi estimar os custos diretos da insuficiência cardíaca na Região Autónoma da Madeira.
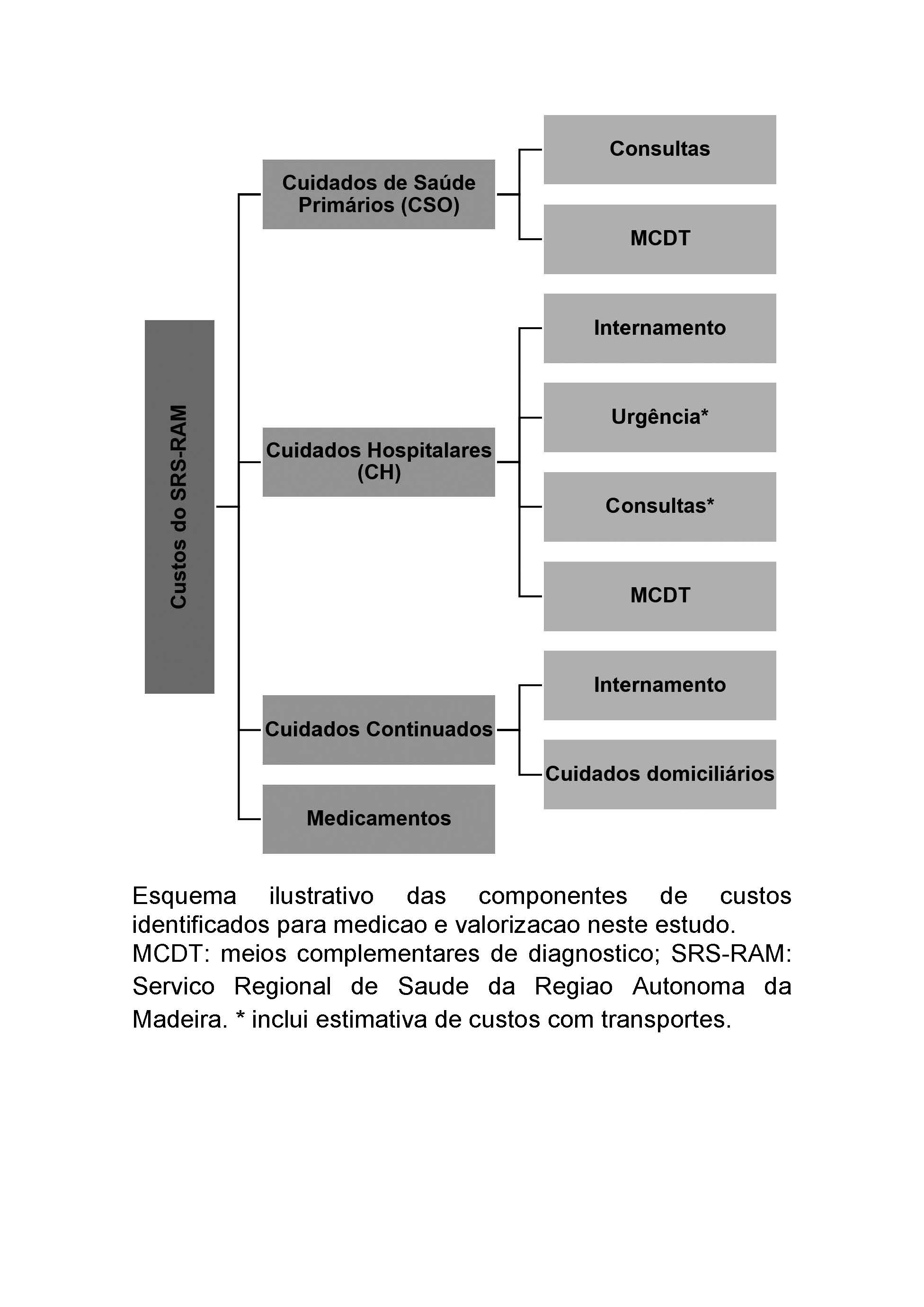
Métodos: Estudo custo-doença, baseado em prevalência,
relativo ao ano 2014, e analisado na perspetiva do sistema de saúde regional. Os internamentos e a utilização da urgência foram identificados pela International Classification of Diseases 9th edition Clinical Modification (ICD-9CM). O número de consultas, exames e medicação foi estimado a partir da literatura. Os custos foram baseados na tabela de preços dos Grupos de Diagnósticos Homogéneos e na tabela de preços do Sistema Regional de Saúde.
Resultados: Estimou-se uma prevalência de 4,93% (9201
indivíduos) para uma população com idade superior a 25
anos. Destes, 4140 sintomáticos e, portanto, consumidores
de recursos. Identificaram-se 426 internamentos por IC, 17
305 consultas médicas de cuidados de saúde primários, 857
episódios de urgência e 6707 consultas médicas hospitalares. O custo direto total foi €4 089 540,10. O custo em cuidados hospitalares (CH) foi a principal rubrica de custos (56%), seguido dos cuidados de saúde primários (23%) e consumo de medicamentos (20%). O custo médio anual por doente foi €987,81.
Conclusão: O custo direto total corresponde a 0,1% do
produto interno bruto da RAM e 1,2% da despesa da saúde
da RAM para o ano de referência. Estes resultados fornecem informação até aqui desconhecida e poderão auxiliar na implementação de modelos e estruturas que promovam a redução das hospitalizações, principal motor de custos diretos.
Downloads
References
Juenger J, Schellberg D, Kraemer S, Haunstetter A, Zugck C, Herzog W, et al. Health related quality of life in patients with congestive heart failure: comparison with other chronic diseases and relation to functional variables. Heart. 2002;87:235-41. doi: 10.1136/heart.87.3.235.
Coelho R, Ramos S, Prata J, Bettencourt P, Ferreira A, Cerqueira-Gomes M. Heart failure and health related quality of life. Clin Pract Epidemiol Ment Health. 2005;1:19. doi: 10.1186/1745-0179-1-19.
Heo S, Lennie TA, Okoli C, Moser DK. Quality of life in patients with heart failure: ask the patients. Heart Lung. 2009;38:100-8. doi: 10.1016/j.hrtlng.2008.04.002.
Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6:606-19.doi: 10.1161/HHF.0b013e318291329a.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129-200. doi: 10.1093/eurheartj/ehw128.
Braunschweig F, Cowie MR, Auricchio A. What are the costs of heart failure? Europace. 2011;13 Suppl 2:ii13-7. doi: 10.1093/europace/eur081.
Najafi F, Jamrozik K, Dobson AJ. Understanding the 'epidemic of heart failure': a systematic review of trends in determinants of heart failure. Eur J Heart Fail. 2009;11:472-9. doi: 10.1093/eurjhf/hfp029.
Roger VL, Weston SA, Redfield MM, Hellermann-Homan JP, Killian J, Yawn BP, et al. Trends in heart failure incidence and survival in a community-based population. JAMA. 2004;292:344-50. doi: 10.1001/jama.292.3.344.
Journath G, Hammar N, Elofsson S, Linnersjö A, Vikström M, Walldius G, et al. Time trends in incidence and mortality of acute myocardial infarction, and all-cause mortality following a cardiovascular prevention program in Sweden. PLoS One. 2015;10:e0140201. doi: 10.1371/journal.pone.0140201.
Fonseca C. Perspetiva para a melhoria do tratamento da insuficiência cardíaca--- um contributo local. Rev Port Cardiol. 2017;36:439–41.
Gouveia MR, Ascenção RM, Fiorentino F, Costa JN, Broeiro-Gonçalves PM, et al. Current costs of heart failure in Portugal and expected increases due to population aging. Rev Port Cardiol. 2020;39:3-11. doi: 10.1016/j.repc.2019.09.006.
Ceia F, Fonseca C, Azevedo I, Mota T, Morais H, Matias F, et al. Epidemiologia da Insuficiência Cardíaca em Cuidados Primários na Região Autónoma da Madeira: o Estudo EPICA-RAM. Rev Port Cardiol. 2005;24:173–89.
Bonow RO, Bennett S, Casey DE Jr, Ganiats TG, Hlatky MA, Konstam MA, et al. ACC/AHA clinical performance measures for adults with chronic heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures (Writing Committee to Develop Heart Failure Clinical Performance Measures) endorsed bym the Heart Failure Society of America. J Am Coll Cardiol. 2005;46:1144-78. doi: 10.1016/j.jacc.2005.07.012.
Blecker S, Paul M, Taksler G, Ogedegbe G, Katz S. Heart failure–associated hospitalizations in the United States. J Am Coll Cardiol. 2013;61:1259-67. doi: 10.1016/j.jacc.2012.12.038.
McCormick N, Lacaille D, Bhole V, Avina-Zubieta JA. Validity of heart failure diagnoses in administrative databases: a systematic review and meta-analysis. PLoS One. 2014;9:e104519. doi: 10.1371/journal.pone.0104519.
Munir MB, Sharbaugh MS, Thoma FW, Nisar MU, Kamran AS, Althouse AD, et al. Trends in hospitalization for congestive heart failure, 1996-2009. Clin Cardiol. 2017;40:109-19. doi: 10.1002/clc.22638.
Quach S, Blais C, Quan H. Administrative data have high variation in validity for recording heart failure. Can J Cardiol. 2010;26:306-12. doi: 10.1016/s0828-282x(10)70438-4.
Marques I, Gomes C, Viamonte S, Ferreira G, Mendonça C. Clínica Multidisciplinar de Insuficiência Cardíaca : Como Implementar Multidisciplinary Heart Failure Clinic : How to Implement. Rev Med Interna. 2017;24:308–17. doi: 10.24950/rspmi/R58/17/2017
Ascencão R, Fiorentino F, Gouveia M, Costa J, Borges P, Broeiro P, et al. Real-world evidence on heart failure: findings from 25 thousand patients in a portuguese primary care database. Eur J Heart Fail. 2017;19:175–6.
Ministério da. Portaria n.o 20/2014 de 29 de Janeiro. Preços a praticar pelo Serviço Nacional de Saúde. [Internet]. Diário da República 2014 p.597–8. Available from: http://diretiva.min-saude.pt/wp-content/uploads/sites/2/2014/08/Portaria-n.o-20-2014-de-20-de-janeiro-–-Tabela-de-preços-a-praticar-pelo-Serviço-Nacional-de-Saúde1.pdf
Ministérios das Finanças e da Administração Pública do Trabalho e da Solidariedade Social e da Saúde. Portaria n.o 262/2015 de 28 de agosto. 2015.
Madeira, Jornal Oficial da Região Autónoma da - I série, no 40 11 de Abril 2003. Resolução n.o 368/2003: Tabela de preços pelos serviços de transporte de doentes prestados ao Serviço Regional de Saúde. 2003.
Rui P, Kang K. National Hospital Ambulatory Medical Care Survey : 2014 Emergency Department Summary Tables. 2014; [accessed Jan 2023] Available from: https://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2014_ed_web_tables.pdf
Cook C, Cole G, Asaria P, Jabbour R, Francis DP. The annual global economic burden of heart failure. Int J Cardiol. 2014;171:368-76. doi: 10.1016/j.ijcard.2013.12.028.
Claes N, Jacobs N, Vijgen J. Impact of heart failure on hospital activity and healthcare costs in Belgium. J Med Econ. 2008;11:71-9. doi:
3111/13696990701672664.
Rydén-Bergsten T, Andersson F. The health care costs of heart failure in Sweden. J Intern Med. 1999;246:275-84. doi: 10.1046/j.1365-
-2796.1999.00520.x.
Szucs TD. The growing healthcare burden of CHF. J Renin Angiotensin Aldosterone Syst. 2000;Suppl 1:2-6. doi: 10.3317/JRAAS.2000.029.
Berry C, Murdoch DR, McMurray JJ. Economics of chronic heart failure. Eur J Heart Fail. 2001;3:283-91. doi: 10.1016/s1388-9842(01)00123-4.
Lesyuk W, Kriza C, Kolominsky-Rabas P. Cost-of-illness studies in heart failure: a systematic review 2004-2016. BMC Cardiovasc Disord. 2018;18:74. doi: 10.1186/s12872-018-0815-3.
Stewart S, Jenkins A, Buchan S, McGuire A, Capewell S, McMurray JJ. The current cost of heart failure to the National Health Service in the UK. Eur J Heart Fail. 2002;4:361-71. doi: 10.1016/s1388-9842(01)00198-2.
Gouveia M, Ascenção R, Fiorentino F, Costa J, Caldeira D, Broeiro-Gonçalves P, et al. The current and future burden of heart failure in Portugal. ESC Heart Fail. 2019;6:254-61. doi: 10.1002/ehf2.12399.
Pérez-Rodríguez G, Brito-Zurita OR, Sistos-Navarro E, Benítez-Aréchiga ZM, Sarmiento-Salazar GL, Vargas-Lizárraga JF. Telemetric monitoring reduces visits to the emergency room and cost of care in patients with chronic heart failure α~. Cirugía Cir. 2015;83:279–85. doi: 10.1016/j.circen.2015.09.016
Mueller TM, Vuckovic KM, Knox DA, Williams RE. Telemanagement of heart failure: a diuretic treatment algorithm for advanced practice nurses. Heart Lung. 2002;31:340-7. doi: 10.1067/mhl.2002.126048.
Sauer J, Rabelo ER, Castro RA, Goldraich L, Rohde LE, Clausell N, et al. Nurses' performance in classifying heart failure patients based on physical exam: comparison with cardiologist's physical exam and levels of N-terminal pro-B-type natriuretic peptide. J Clin Nurs. 2010;19:3381-9. doi: 10.1111/j.1365-2702.2010.03403.x.
Fonseca C, Brito D, Cernadas R, Ferreira J, Franco F, Rodrigues T, et al. Pela melhoria do tratamento da insuficiência cardíaca em Portugal – documento de consenso. Rev Port Cardiol. 2017;36:1–8. doi: 10.1016/j.repc.2016.10.006
Downloads
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2024 Internal Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.





