Sglt2 Inhibitor: An Antidiabetic, Cardioenhancer, Renoprotector…or the Internist's Elixir?
Revisão Narrativa - Uma narrativa baseada na história e na prova
DOI:
https://doi.org/10.24950/rspmi.2183Keywords:
Diabetes Mellitus, Type 2/drug therapy, Heart Failure/drug therapy, Internal Medicine, Renal Insufficiency, Chronic/drug therapy, Sodium-Glucose Transporter 2 Inhibitors/ therapeutic useAbstract
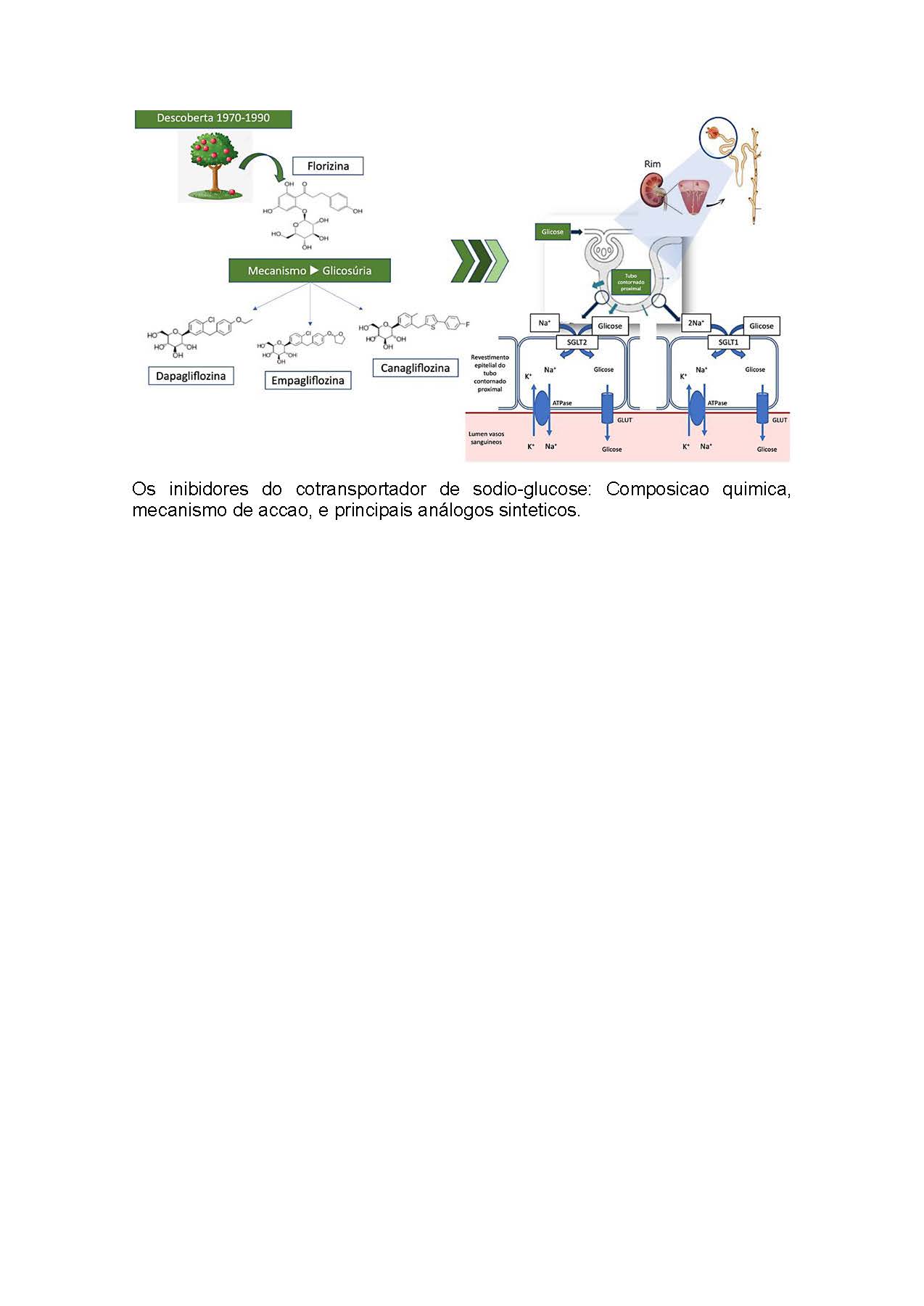
This review article addresses the history, underlying evidence, proposed mechanisms, and clinical implication of
sodium glucose cotransporter type 2 inhibitors (SGLT2i),
framing them from the perspective of the general practitioner internist of the present decade.
The sodium glucose cotransporter inhibitors, once
identified in the apple tree root bark but with no obvious
therapeutic purpose, were initially developed as another hypoglycemic agent. Recently, its use has undergone a reversal. Large randomized controlled clinical trials revealed: first drug class to improve cardiovascular outcomes and mortality in type 2 diabetes; one more prognosis-modifying class in heart failure; first class with clear benefit in prognosis and even mortality in chronic kidney disease. The mechanisms are still not completely understood, but hypotheses include a diuretic effect and metabolism modulation.
Internal Medicine, as a differentiating generalist specialty,
is par excellence able to deal with the all spectrum use of SGLT2i.
Downloads
References
White JR. Apple trees to sodium glucose co-transporter inhibitors: a review of SGLT2 inhibition. Clin Diabetes. 2010;28: 5-10. doi: 10.2337/diaclin.28.1.5
Ehrenkranz JR, Lewis NG, Kahn CR, Roth J. Phlorizin: a review. Diabetes Metab Res Rev. 2005;21:31-8. doi: 10.1002/dmrr.532
Lee WS, Kanai Y, Wells RG, Hediger MA. The high affinity NA/glucose cotransporter: re-evaluation and distribution of expression. J Biol Chem. 1994; 269:12032–9. doi: 10.1002/dmrr.532
Abdul-Ghani MA, Norton L, DeFronzo RA. Role of sodium-glucose cotransporter 2 (SGLT 2) inhibitors in the treatment of type 2 diabetes. Endocr Rev. 2011;32:515-31. doi: 10.1210/er.2010-0029
UK Prospective Diabetes Study (UKPDS) Group et al. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet. 1998;352: 854-65. doi: 10.1016/S0140-6736(98)07037-8
Morrish NJ, Wang SL, Stevens LK, Fuller JH, Keen H, WHO Multinational Study Group, et al. Mortality and causes of death in the WHO Multinational Study of Vascular Disease in Diabetes. Diabetologia. 2001;44: S14-S21. doi: 10.1007/PL00002934
Selvin E, Bolen S, Yeh HC, Wiley C, Wilson LM, Marinopoulos SS, et al. Cardiovascular outcomes in trials of oral diabetes medications: a systematic review. Arch Intern Med. 2008;168.19: 2070-80. doi: 10.1001/archinte.168.19.2070
Guidance for Industry Diabetes Mellitus — Evaluating Cardiovascular Risk in New Antidiabetic Therapies to Treat Type 2 Diabetes. U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research [consultado 2023 Jul 10]. Available at: http://www.sefap.it/servizi_lineeguida_200901/8576fnl.pdf.
Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373: 2117-28. doi: 10.1056/NEJMoa1504720
Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377: 644-57. doi: 10.1056/NEJMoa1611925.
Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019;380: 347-57. doi: 10.1056/NEJMoa1812389
Mahaffey KW, Jardine MJ, Bompoint S, Cannon CP, Neal B, Heerspink HJL, et al. Canagliflozin and cardiovascular and renal outcomes in type 2 diabetes mellitus and chronic kidney disease in primary and secondary cardiovascular prevention groups: results from the randomized CREDENCE trial. Circulation. 2019;140: 739-50. doi: 10.1161/CIRCULATIONAHA.119.042007.
Cannon CP, Pratley R, Dagogo-Jack S, Mancuso J, Huyck S, Masiukiewicz U, et al. Cardiovascular outcomes with ertugliflozin in type 2 diabetes. N Engl J Med. 2020;383: 1425-35. doi: 10.1056/NEJMoa2004967.
Bhatt DL, Szarek M, Steg G, Cannon CP, Leiter LA, McGuire DK, et al. Sotagliflozin in patients with diabetes and recent worsening heart failure. N Engl J Med. 2021; 384: 117-28. doi: 10.1056/NEJMoa2030183
Bhatt DL, Szarek M, Pitt B, Cannon CP, Leiter LA, McGuire DK, et al. Sotagliflozin in patients with diabetes and chronic kidney disease. N Engl J Med. 2021;384: 129-39. doi: 10.1056/NEJMoa2030186
McMurray JJV, Solomon SD, Inzucchi SE, Køber L, Kosiborod MN, Martinez FA, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381: 1995-2008. doi: 10.1056/NEJMoa1911303
Packer M, Anker SD, Butler J, Filippatos G, Pocock SJ, Carson P, et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N Engl J Med. 2020;383: 1413-24. doi: 10.1056/NEJMoa2022190
Heerspink HJL, Stefánsson BV, Correa-Rotter R, Chertow GM, Greene T, Hou FF, et al. Dapagliflozin in patients with chronic kidney disease. N Engl J Med. 2020;383: 1436-46. doi: 10.1056/NEJMoa2024816
Anker SD, Butler J, Filippatos G, Ferreira JP, Bocchi E, Böhm M, et al. Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med. 2021;385: 1451-61. doi: 10.1056/NEJMoa2107038
Bakris GL, Agarwal R, Anker SD, Pitt B, Ruilope LM, Rossing P, et al. Effect of finerenone on chronic kidney disease outcomes in type 2 diabetes N Engl J Med. 2020;383: 2219-29. doi: 10.1056/NEJMoa2025845
Pitt B, Filippatos G, Agarwal R, Anker SD, Bakris GL, Rossing P, et al. Cardiovascular events with finerenone in kidney disease and type 2 diabetes. N Engl J Med. 2021; 385: 2252-63. doi: 10.1056/NEJMoa2110956
EMPA-KIDNEY Collaborative Group. Empagliflozin in patients with chronic kidney disease. N Engl J Med. 2023;388: 117-27. doi: 10.1056/NEJMoa2204233
Solomon SD, McMurray JJV, Claggett B, Boer RA, DeMets D, Hernandez AF, et al. Dapagliflozin in heart failure with mildly reduced or preserved ejection fraction. N Engl J Med. 2022;387: 1089-98. doi: 10.1056/NEJMoa2206286
Stapff MP. Using real world data to assess cardiovascular outcomes of two antidiabetic treatment classes. World J Diabetes. 2018;9:252-7. doi: 10.4239/wjd.v9.i12.252.
D'Andrea E, Wexler DJ, Kim SC, Paik JM, Alt E, Patorno E. Comparing Effectiveness and Safety of SGLT2 Inhibitors vs DPP-4 Inhibitors in Patients With Type 2 Diabetes and Varying Baseline HbA1c Levels. JAMA Intern Med. 2023;183:242-54. doi: 10.1001/jamainternmed.2022.6664. .
Vasconcelos C, Vilar Santos S, Vilela A, de Faria R, Reis Á. Inibidores da SGLT2 no tratamento da diabetes mellitus e a sua influência no peso, a experiência de uma unidade de saúde portuguesa. Rev Port Med Geral Fam. 2023;39:187–94. doi:10.32385/rpmgf.v39i3.13641
Perrone-Filardi P, Avogaro A, Bonora E, Colivicchi F, Fioretto P, Maggioni AP, et al. Mechanisms linking empagliflozin to cardiovascular and renal protection. Int J Cardiol 2017;241: 450-6. doi: 10.1016/j.ijcard.2017.03.089
Verma S and McMurray JJV. SGLT2 inhibitors and mechanisms of cardiovascular benefit: a state-of-the-art review. Diabetologia. 2018;61: 2108-17. doi: 10.1007/s00125-018-4670-7
de la Espriella R, Bayés-Genís A, Morillas H, Bravo R, Vidal V, Núñez, et al. Renal function dynamics following co-administration of sacubitril/valsartan and empagliflozin in patients with heart failure and type 2 diabetes. ESC Heart Failure. 2020;7: 3792-800. doi: 10.1002/ehf2.12965
Griffin M, Rao VS, Ivey-Miranda J, Fleming J, Mahoney D, Maulion C, et al. Empagliflozin in Heart Failure: Diuretic and Cardio-Renal Effects. Circulation. 2020;142: 1028-39. doi: 10.1161/CIRCULATIONAHA.120.045691
Sano M, Goto S. Possible mechanism of hematocrit elevation by sodium glucose cotransporter 2 inhibitors and associated beneficial renal and cardiovascular effects. Circulation. 2019;139: 1985-7.
Lehrke M. SGLT2 Inhibition: Changing What Fuels the Heart. J Am Coll Cardiol. 2019;73:1945-7. doi: 10.1016/j.jacc.2019.02.023.
Sato, Takao, et al. "The effect of dapagliflozin treatment on epicardial adipose tissue volume." Cardiovasc Diabet. 2018;17:6. doi: 10.1161/CIRCULATIONAHA. 118.038881
Packer M. Do sodium-glucose co-transporter-2 inhibitors prevent heart failure with a preserved ejection fraction by counterbalancing the effects of leptin? A novel hypothesis. Diabetes Obes Metab. 2018;20: 1361-6. doi: 10.1111/dom.13229
Santos-Gallego CG, Requena-Ibanez JA, San Antonio R, Ishikawa K, Watanabe S, Picatoste B, et al. Empagliflozin ameliorates adverse left ventricular remodeling in nondiabetic heart failure by enhancing myocardial energetics. J Am Coll Cardiol. 2019;73: 1931-44. doi: 10.1016/j.jacc.2019.01.056
Uthman L, Baartscheer A, Schumacher CA, Fiolet JW, Kuschma MC, Hollmann MW, et al. Direct cardiac actions of sodium glucose cotransporter 2 inhibitors target pathogenic mechanisms underlying heart failure in diabetic patients. Front Physioly. 2018;9: 1575. doi: 10.3389/fphys.2018.01575
Goldman A, Fishman B, Twig G, Raschi E, Cukierman-Yaffe T, Moshkovits Y, et al. The real-world safety profile of sodium-glucose co-transporter-2 inhibitors among older adults (≥ 75 years): a retrospective, pharmacovigilance study. Cardiovasc Diabetol. 2023;22:16. doi: 10.1186/s12933-023-01743-5.
Fu EL, D'Andrea E, Wexler DJ, Patorno E, Paik JM. Safety of Sodium-Glucose Cotransporter-2 Inhibitors in Patients with CKD and Type 2 Diabetes: Population-Based US Cohort Study. Clin J Am Soc Nephrol. 2023;18:592–601. doi: 10.2215/CJN.0000000000000115.
Vardeny O, Vaduganathan M. Practical guide to prescribing sodium-glucose cotransporter 2 inhibitors for cardiologists. JACC Hear Fail. 2019;7:169–72. doi: 10.1016/j.jchf.2018.11.013.
Marques I, Gomes C, Viamonte S, Ferreira G, Mendonça C. Clínica Multidisciplinar de Insuficiência Cardíaca: Como Implementar. Med Intern. 2017;24:308-17.
Bettencour P, Pimenta J, Araújo I, Marques I, Lourenço C, Sarmento PM. Checklist para A Pré-Alta de Internamento por Insuficiência Cardíaca. Med Intern. 2021;28:76-81.
Tolkien JRR. The Lord of the Rings: The Two Towers. London: Harper Collins Publishers; 2012.
Brito D, Bettencourt P, Carvalho D, Ferreira J, Fontes-Carvalho R, Franco F, et al. Sodium-Glucose Co-transporter 2 Inhibitors in the Failing Heart: a Growing Potential. Cardiovasc Drugs Ther. 2020;34:419-36. doi: 10.1007/s10557-020-06973-3.
Downloads
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2024 Internal Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright (c) 2023 Medicina Interna





