Metabolic Dysfunction-Associated Steatotic Liver Disease: An Update on Screening and Therapeutic Options
Doença Hepática Esteatótica Associada a Disfunção Metabólica: Uma Atualização do Rastreio e Opções Terapêuticas
DOI:
https://doi.org/10.24950/rspmi.2522Keywords:
Diabetes Mellitus, Type 2, Fatty Liver, Metabolic Syndrome, Non-alcoholic Fatty Liver DiseaseAbstract
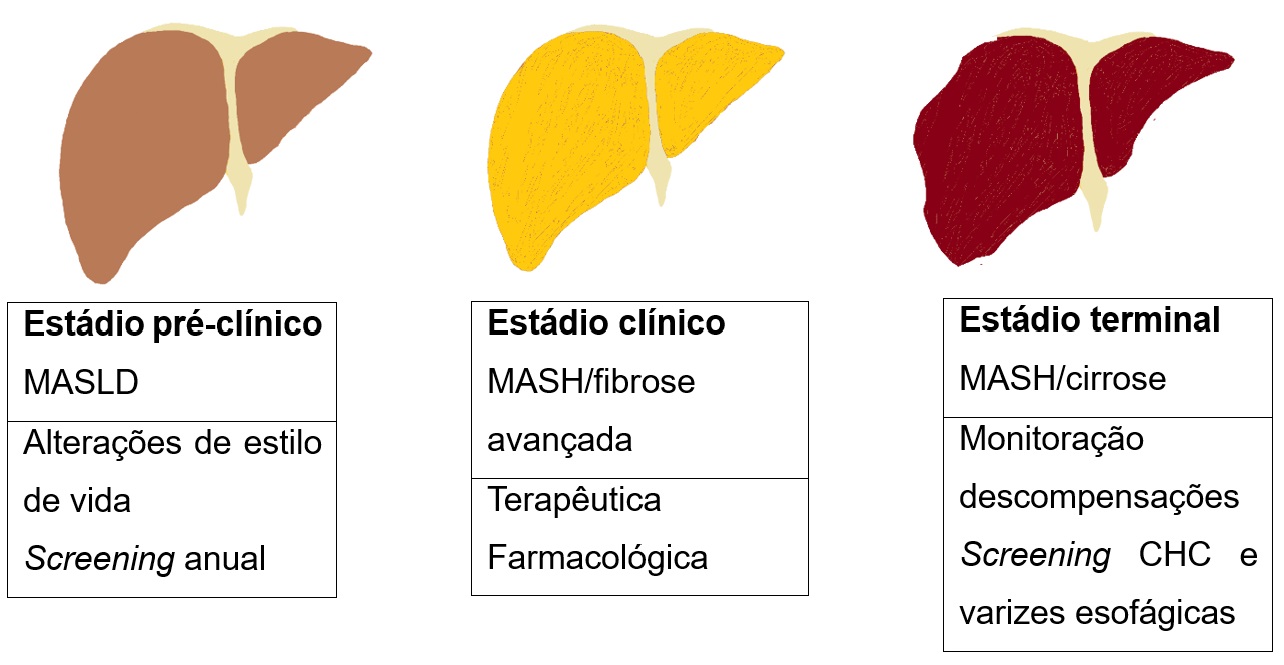
Metabolic dysfunction-associated steatotic liver disease (MASLD) is one of the most common forms of chronic liver disease, particularly associated with obesity and type 2 diabetes mellitus. The prevalence has been increasing in recent years, currently affecting around 25% of the world's population. The hallmark of its pathophysiology lies in insulin resistance and the accumulation of fat inside hepatocytes. Several clinical scores allow cost-effective screening, such as FIB-4 and NFS. Although it is considered the gold standard, liver biopsy can often be avoided by using hepatic elastography. Numerous drugs used in diabetes have therapeutic potential in metabolic dysfunction-associated steatotic liver disease, with the most studied class being GLP-1 receptor agonists. The bidirectional pathophysiological association between metabolic dysfunction-associated steatotic liver disease and diabetes will enable the development of this field and the emergence of new therapies
Downloads
References
Sberna AL, Bouillet B, Rouland A, Brindisi MC, Nguyen A, Mouillot T, et al. European Association for the Study of the Liver (EASL), European Association for the Study of Diabetes (EASD) and European Association for the Study of Obesity (EASO) clinical practice recommendations for the management of non-alcoholic fatty liver disease: evaluation of their application in people with Type 2 diabetes. Diabet Med. 2018;35:368-75. doi: 10.1111/dme.13565.
Dewidar B, Kahl S, Pafili K, Roden M. Metabolic liver disease in diabetes - From mechanisms to clinical trials. Metabolism. 2020;111S:154299. doi: 10.1016/j.metabol.2020.154299.
Gancheva S, Bierwagen A, Kaul K, Herder C, Nowotny P, Kahl S, et al. Variants in Genes Controlling Oxidative Metabolism Contribute to Lower Hepatic ATP Independent of Liver Fat Content in Type 1 Diabetes. Diabetes. 2016;65:1849-57. doi: 10.2337/db16-0162.
Rinella ME, Lazarus JV, Ratziu V, Francque SM, Sanyal AJ, Kanwal F, et al. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. Ann Hepatol. 2024;29:101133. doi: 10.1016/j.aohep.2023.101133.
Ratziu V, Boursier J; AFEF Group for the Study of Liver Fibrosis. Confirmatory biomarker diagnostic studies are not needed when transitioning from NAFLD to MASLD. J Hepatol. 2024;80:e51-e52. doi: 10.1016/j.jhep.2023.07.017.
Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73-84. doi: 10.1002/hep.28431.
Tilg H, Moschen AR, Roden M. NAFLD and diabetes mellitus. Nat Rev Gastroenterol Hepatol. 2017;14:32-42. doi: 10.1038/nrgastro.2016.147.
Manka PP, Kaya E, Canbay A, Syn WK. A Review of the Epidemiology, Pathophysiology, and Efficacy of Anti-diabetic Drugs Used in the Treatment of Nonalcoholic Fatty Liver Disease. Dig Dis Sci. 2021;66:3676-88. doi: 10.1007/s10620-021-07206-9.
Stepanova M, Rafiq N, Makhlouf H, Agrawal R, Kaur I, Younoszai Z, et al. Predictors of all-cause mortality and liver-related mortality in patients with non-alcoholic fatty liver disease (NAFLD). Dig Dis Sci. 2013;58:3017-23. doi: 10.1007/s10620-013-2743-5.
Dougherty JA, Guirguis E, Thornby KA. A Systematic Review of Newer Antidiabetic Agents in the Treatment of Nonalcoholic Fatty Liver Disease. Ann Pharmacother. 2021;55:65-79. doi: 10.1177/1060028020935105.
Pouwels S, Sakran N, Graham Y, Leal A, Pintar T, Yang W, et al. Non-alcoholic fatty liver disease (NAFLD): a review of pathophysiology, clinical management and effects of weight loss. BMC Endocr Disord. 2022;22:63. doi: 10.1186/s12902-022-00980-1.
Ma X, Liu S, Zhang J, Dong M, Wang Y, Wang M, Xin Y. Proportion of NAFLD patients with normal ALT value in overall NAFLD patients: a systematic review and meta-analysis. BMC Gastroenterol. 2020;20:10. doi: 10.1186/s12876-020-1165-z.
Corey KE, Klebanoff MJ, Tramontano AC, Chung RT, Hur C. Screening for nonalcoholic steatohepatitis in individuals with type 2 diabetes: a cost-effectiveness analysis. Dig Dis Sci. 2016;61:2108-17. doi: 10.1007/s10620-016-4044-2.
Noureddin M, Jones C, Alkhouri N, Gomez EV, Dieterich DT, Rinella ME, et al. Screening for Nonalcoholic Fatty Liver Disease in Persons with Type 2 Diabetes in the United States Is Cost-effective: A Comprehensive Cost-Utility Analysis. Gastroenterology. 2020;159:1985-7.e4. doi: 10.1053/j.gastro.2020.07.050.
Vallet-Pichard A, Mallet V, Nalpas B, Verkarre V, Nalpas A, Dhalluin-Venier V, et al. FIB-4: an inexpensive and accurate marker of fibrosis in HCV infection. comparison with liver biopsy and fibrotest. Hepatology. 2007;46:32-6. doi: 10.1002/hep.21669.
Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, et al. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67:328-57. doi: 10.1002/hep.29367.
Eslam M, Sarin SK, Wong VW, Fan JG, Kawaguchi T, Ahn SH, et al. The Asian Pacific Association for the Study of the Liver clinical practice guidelines for the diagnosis and management of metabolic associated fatty liver disease. Hepatol Int. 202014:889-919. doi: 10.1007/s12072-020-10094-2.
Petta S, Wong VW, Cammà C, Hiriart JB, Wong GL, Marra F, et al. Improved noninvasive prediction of liver fibrosis by liver stiffness measurement in patients with nonalcoholic fatty liver disease accounting for controlled attenuation parameter values. Hepatology. 2017;65:1145-55. doi: 10.1002/hep.28843.
Jafarov F, Kaya E, Bakir A, Eren F, Yilmaz Y. The diagnostic utility of fibrosis-4 or nonalcoholic fatty liver disease fibrosis score combined with liver stiffness measurement by fibroscan in assessment of advanced liver fibrosis: a biopsy-proven nonalcoholic fatty liver disease study. Eur J Gastroenterol Hepatol. 2020;32:642-9. doi: 10.1097/MEG.0000000000001573.
Angulo P, Hui JM, Marchesini G, Bugianesi E, George J, Farrell GC, et al. The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology. 2007;45:846-54. doi: 10.1002/hep.21496.
Pandyarajan V, Gish RG, Alkhouri N, Noureddin M. Screening for Nonalcoholic Fatty Liver Disease in the Primary Care Clinic. Gastroenterol Hepatol. 2019;15:357-65.
Newsome PN, Sasso M, Deeks JJ, Paredes A, Boursier J, Chan WK, et al. FibroScan-AST (FAST) score for the non-invasive identification of patients with non-alcoholic steatohepatitis with significant activity and fibrosis: a prospective derivation and global validation study. Lancet Gastroenterol Hepatol. 2020;5:362-73. doi: 10.1016/S2468-1253(19)30383-8.
Sumida Y, Yoneda M, Ogawa Y, Yoneda M, Okanoue T, Nakajima A. Current and new pharmacotherapy options for non-alcoholic steatohepatitis. Expert Opin Pharmacother. 2020;21:953-67. doi: 10.1080/14656566.2020.1744564.
Brunton SA. The potential role of sodium glucose co-transporter 2 inhibitors in the early treatment of type 2 diabetes mellitus. Int J Clin Pract. 2015;69:1071-87. doi: 10.1111/ijcp.12675.
Akuta N, Kawamura Y, Watanabe C, Nishimura A, Okubo M, Mori Y, et al Impact of sodium glucose cotransporter 2 inhibitor on histological features and glucose metabolism of non-alcoholic fatty liver disease complicated by diabetes mellitus. Hepatol Res. 2019;49:531-9. doi: 10.1111/hepr.13304.
Lee KW, Devaraj NK, Ching SM, Veettil SK, Hoo FK, Deuraseh I, et al. Effect of SGLT-2 inhibitors on non-alcoholic fatty liver disease among patients with type 2 diabetes mellitus: systematic review with meta-analysis and trial sequential analysis of randomized clinical trials. Oman Med J. 2021;36:e273. doi: 10.5001/omj.2021.62.
Ranjbar G, Mikhailidis DP, Sahebkar A. Effects of newer antidiabetic drugs on nonalcoholic fatty liver and steatohepatitis: Think out of the box! Metabolism. 2019;101:154001. doi: 10.1016/j.metabol.2019.154001.
Gastaldelli A, Cusi K. From NASH to diabetes and from diabetes to NASH: Mechanisms and treatment options. JHEP Rep. 2019;1:312-28. doi: 10.1016/j.jhepr.2019.07.002.
Fan H, Pan Q, Xu Y, Yang X. Exenatide improves type 2 diabetes concomitant with non-alcoholic fatty liver disease. Arq Bras Endocrinol Metabol. 2013;57:702-8. doi: 10.1590/s0004-27302013000900005.
Dutour A, Abdesselam I, Ancel P, Kober F, Mrad G, Darmon P, et al. Exenatide decreases liver fat content and epicardial adipose tissue in patients with obesity and type 2 diabetes: a prospective randomized clinical trial using magnetic resonance imaging and spectroscopy. Diabetes Obes Metab. 2016;18:882-91. doi: 10.1111/dom.12680.
Ohki T, Isogawa A, Iwamoto M, Ohsugi M, Yoshida H, Toda N, et al. The effectiveness of liraglutide in nonalcoholic fatty liver disease patients with type 2 diabetes mellitus compared to sitagliptin and pioglitazone. ScientificWorldJournal. 2012;2012:496453. doi: 10.1100/2012/496453.
Zhang Z, Qi Y, Kong W, Jin Q, Wang X, Dong Y, et al. Efficacy and Clinical Value of Liraglutide for Treatment of Diabetes Mellitus Complicated by Non-Alcoholic Fatty Liver Disease. Med Sci Monit. 2018;24:7399-404. doi: 10.12659/MSM.911062.
Petit JM, Cercueil JP, Loffroy R, Denimal D, Bouillet B, Fourmont C, et al. Effect of liraglutide therapy on liver fat content in patients with inadequately controlled type 2 diabetes: The Lira-NAFLD Study. J Clin Endocrinol Metab. 2017;102:407-15. doi: 10.1210/jc.2016-2775.
Armstrong MJ, Gaunt P, Aithal GP, Barton D, Hull D, Parker R, et al. Liraglutide safety and efficacy in patients with non-alcoholic steatohepatitis (LEAN): a multicentre, double-blind, randomised, placebo-controlled phase 2 study. Lancet. 2016;387:679-90. doi: 10.1016/S0140-6736(15)00803-X.
Matikainen N, Söderlund S, Björnson E, Pietiläinen K, Hakkarainen A, Lundbom N, et al. Liraglutide treatment improves postprandial lipid metabolism and cardiometabolic risk factors in humans with adequately controlled type 2 diabetes: A single-centre randomized controlled study. Diabetes Obes Metab. 2019;21:84-94. doi: 10.1111/dom.13487.
Seko Y, Sumida Y, Tanaka S, Mori K, Taketani H, Ishiba H, et al. Effect of 12-week dulaglutide therapy in Japanese patients with biopsy-proven non-alcoholic fatty liver disease and type 2 diabetes mellitus. Hepatol Res. 2017;47:1206-11. doi: 10.1111/hepr.12837.
Cusi K, Sattar N, García-Pérez LE, Pavo I, Yu M, Robertson KE, et al. Dulaglutide decreases plasma aminotransferases in people with Type 2 diabetes in a pattern consistent with liver fat reduction: a post hoc analysis of the AWARD programme. Diabet Med. 2018;35:1434-9. doi: 10.1111/dme.13697.
Newsome PN, Buchholtz K, Cusi K, Linder M, Okanoue T, Ratziu V, et al. A Placebo-Controlled Trial of Subcutaneous Semaglutide in Nonalcoholic Steatohepatitis. N Engl J Med. 2021;384:1113-24. doi: 10.1056/NEJMoa2028395.
Marso SP, Bain SC, Consoli A, Eliaschewitz FG, Jódar E, Leiter LA, et al Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes. N Engl J Med. 2016;375:1834-44. doi: 10.1056/NEJMoa1607141.
Pratley RE, Aroda VR, Lingvay I, Lüdemann J, Andreassen C, Navarria A, et al. Semaglutide versus dulaglutide once weekly in patients with type 2 diabetes (SUSTAIN 7): a randomised, open-label, phase 3b trial. Lancet Diabetes Endocrinol. 2018;6:275-86. doi: 10.1016/S2213-8587(18)30024-X.
Hedrington MS, Davis SN. Oral semaglutide for the treatment of type 2 diabetes. Expert Opin Pharmacother. 2019;20:133-41. doi: 10.1080/14656566.2018.1552258.
Forzano I, Varzideh F, Avvisato R, Jankauskas SS, Mone P, Santulli G. Tirzepatide: A Systematic Update. Int J Mol Sci. 2022;23:14631. doi: 10.3390/ijms232314631.
Rosenstock J, Wysham C, Frías JP, Kaneko S, Lee CJ, Fernández Landó L, et al. Efficacy and safety of a novel dual GIP and GLP-1 receptor agonist tirzepatide in patients with type 2 diabetes (SURPASS-1): a double-blind, randomised, phase 3 trial. Lancet. 2021;398:143-55. doi: 10.1016/S0140-6736(21)01324-6.
Hartman ML, Sanyal AJ, Loomba R, Wilson JM, Nikooienejad A, Bray R, et al. Effects of novel dual GIP and GLP-1 receptor agonist tirzepatide on biomarkers of nonalcoholic steatohepatitis in patients with type 2 diabetes. diabetes care. 2020;43:1352-5. doi: 10.2337/dc19-1892.
Bril F, Kalavalapalli S, Clark VC, Lomonaco R, Soldevila-Pico C, Liu IC, et al. Response to Pioglitazone in Patients With Nonalcoholic Steatohepatitis With vs Without Type 2 Diabetes. Clin Gastroenterol Hepatol. 2018;16:558-66.e2. doi: 10.1016/j.cgh.2017.12.001.
Gawrieh S, Noureddin M, Loo N, Mohseni R, Awasty V, Cusi K, et al. Saroglitazar, a PPAR-α/γ Agonist, for Treatment of NAFLD: A Randomized Controlled Double-Blind Phase 2 Trial. Hepatology. 2021;74:1809-24. doi: 10.1002/hep.31843.
Cusi K, Orsak B, Bril F, Lomonaco R, Hecht J, Ortiz-Lopez C, et al. Long-term pioglitazone treatment for patients with nonalcoholic steatohepatitis and prediabetes or type 2 diabetes mellitus: a randomized trial. Ann Intern Med. 2016;165:305-15. doi: 10.7326/M15-1774.
Tokushige K, Ikejima K, Ono M, Eguchi Y, Kamada Y, Itoh Y, et al. Evidence-based clinical practice guidelines for nonalcoholic fatty liver disease/nonalcoholic steatohepatitis 2020. Hepatol Res. 2021;51:1013-25. doi: 10.1111/hepr.13688.
Downloads
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2024 Internal Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Copyright (c) 2023 Medicina Interna





